Megakaryocytes (MKs) are large, polyploid platelet precursor cells that primarily reside within the bone marrow. Recent advances revealed that in addition to platelet production, MKs contribute to immunity and maintenance of bone marrow homeostasis, raising the question of whether these functions are hijacked in disease. One hallmark of primary and secondary myelofibrosis (MF), subsets of myeloproliferative neoplasms, is the accumulation of aberrant, immature MKs in the bone marrow. These release pro-fibrotic cytokines such as transforming growth factor β1 (TGFβ1) and interleukin 1β (IL1β) into the bone marrow, thus inducing fibrotic alterations that ultimately cause pancytopenia - the major cause of mortality in patients with MF. While current treatment strategies in MF aim to prevent MK proliferation and correct the differentiation defects, a direct targeting of cytokine release from MKs has not yet been explored. Recently, unconventional secretion of TGFβ1 and IL1β via secretory autophagy, a secretion pathway driven by the fusion of autophagosomes with the plasma membrane, has been shown to occur in other cell types. We therefore hypothesize that MKs may preferentially utilize secretory autophagy for cytokine release and that inhibiting autophagosome formation might therefore slow fibrosis progression in vivo.
Previous studies suggested that TGFβ1 is stored within specialized α-granules in MKs. To test this, we cultured murine MKs and determined TGFβ1 co-localization with different α-granule proteins by super-resolution confocal microscopy. However, while we did not identify any correlation between TGFβ1 and α-granules, we found that TGFβ1 strongly co-localized with the autophagy marker light chain (LC) 3B, supporting a potential role for secretory autophagy. To investigate this, we disrupted secretory autophagy by inhibiting the GTPase RhoA and its downstream effector Rho kinase (ROCK), which were previously shown to promote autophagosome formation. Treatment of MKs with inhibitors of autophagy or RhoA/ROCK markedly reduced TGFβ1 secretion in vitro and led to intracellular accumulation of TGFβ1. Taken together, these data suggest that TGFβ1 is secreted by MKs via secretory autophagy.
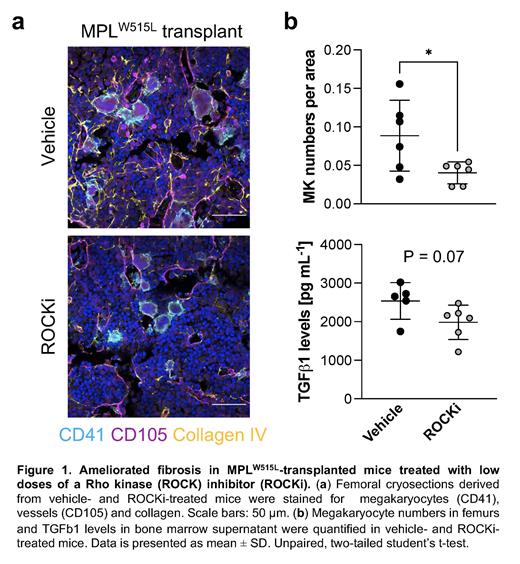
To examine whether secretory autophagy in MKs contributes to disease pathogenesis in vivo, we employed an MPL W515L-driven transplant model. Basal autophagy measured by LC3B conversion and RhoA protein levels were increased in platelets derived from mice with MPL W515L-driven MF. Conditional deletion of the essential autophagy gene Atg5 from the hematopoietic system ( Mx1-Cre+; Atg5fl/fl mice) prevented leukocytosis, MK clustering and aberrant TGFβ1 secretion in the MPL W515L-driven transplant model, indicating that autophagy promotes the initiation of MF. Furthermore, MPL W515L-transplanted mice treated with a low-dose ROCK inhibitor (ROCKi) - several of which are FDA-approved - reduced MK clustering and fibrosis in spleens and femurs of treated mice (Figure 1a, b). To further verify our data, we utilized a second preclinical mouse model of MF - a knockout mouse lacking the inhibitory MK receptor G6b-B ( Mpig6b -/-), which exhibits thrombocytopenia, MK clustering and MF. In line with our previous findings, conditional deletion of Rhoa in MK lineage cells in Pf4-Cre+; Rhoafl/fl; Mpig6b -/- mice normalized TGFβ1 levels within the bone marrow and protected against the development of fibrosis in bone marrow and spleen. In ongoing work, ROCK inhibitors are further being tested in higher doses alone or in combination with the JAK2 inhibitor ruxolitinib.
Overall, our data suggest that TGFβ1 secretion is uncoupled from conventional granule secretion in MKs and is instead dependent on RhoA/autophagy signaling pathways. Targeting these pathways in aberrant MKs represents a new potential therapeutic target in the treatment of MF.
Disclosures
No relevant conflicts of interest to declare.